When a person is taken into custody under the mental health law in Florida and sent for an involuntary psychiatric examination it can be very scary for them and their friends and family. Commonly referred to as a “Baker Act” the initiation of an involuntary exam, what that means and what rights are accorded to a person is often not known and understood.
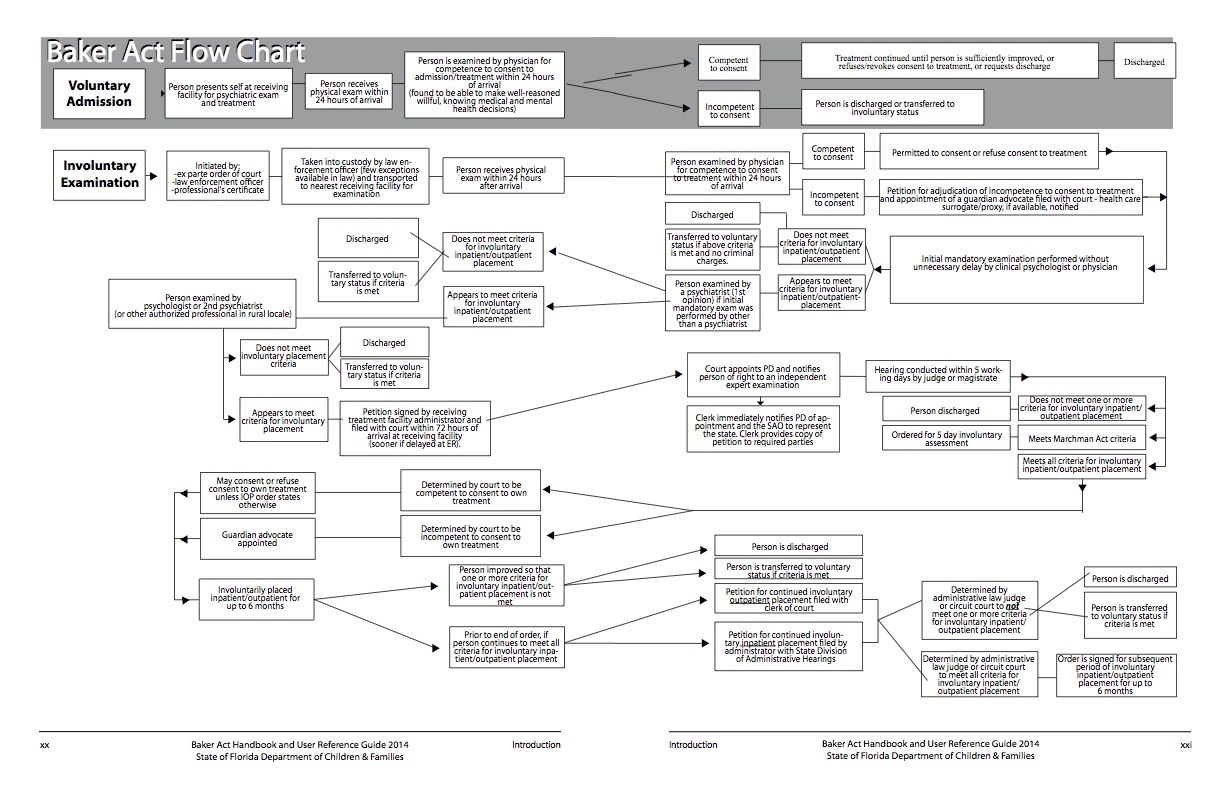
The information below and the flow chart on this page are designed to help anyone better understand the process.
NOTE: The mental health law in Florida was amended in 2017 to offer better protection for minors and the flow chart has not yet been updated to reflect this change.
Question: What are the criteria for an involuntary examination, a Baker Act?
Answer: A person may be taken to a receiving facility (psychiatric ward) for involuntary examination if there is reason to believe that the person has a mental illness and because of his or her mental illness: (a)1.The person has refused voluntary examination after conscientious explanation and disclosure of the purpose of the examination; or 2. The person is unable to determine for himself or herself whether examination is necessary; and (b)1.Without care or treatment, the person is likely to suffer from neglect or refuse to care for himself or herself; such neglect or refusal poses a real and present threat of substantial harm to his or her well-being; and it is not apparent that such harm may be avoided through the help of willing family members or friends or the provision of other services; or 2.There is a substantial likelihood that without care or treatment the person will cause serious bodily harm to himself or herself or others in the near future, as evidenced by recent behavior.
Question: How long may a person be held for involuntary examination under the Baker Act?
Answer: An adult may be held up to 72 hours for an involuntary examination. However the examination period for a minor, anyone 17 or younger, is 12 hours. Specifically the examination for a child “shall be initiated within 12 hours after the patient’s arrival at the facility.”
If the examination period for an adult or a minor has ended then one of the following actions must be taken:
- The patient shall be released, unless he or she is charged with a crime, in which case the patient shall be returned to the custody of a law enforcement officer;
- The patient shall be released for voluntary outpatient treatment;
- The patient, unless he or she is charged with a crime, shall be asked to give express and informed consent to placement as a voluntary patient and, if such consent is given, the patient shall be admitted as a voluntary patient; or
- A petition for involuntary services shall be filed in the circuit court if inpatient treatment is deemed necessary. This is the start of a possible involuntary psychiatric commitment.
NOTE: You do not need to sign yourself in as voluntary in order to be discharged! If the examination period is over and you or your loved one do not want voluntary treatment then by law discharge is the next step unless a crime is involved.
If the examination period ends on a weekend or a holiday then no later than the next working day the above must be done.
Question: When does a patient need to be examined by a health practitioner?
Answer: Florida Statute 394.459 Rights of patients, Section (2) RIGHT TO TREATMENT, Subsection (c) states:
“(c) Each person who remains at a receiving or treatment facility for more than 12 hours shall be given a physical examination by a health practitioner authorized by law to give such examinations, within 24 hours after arrival at such facility.”
It is important to understand that according to the Florida Administrative Code 65E-5.160 Right to Treatment that this examination must include a determination that abnormalities of thought, mood or behavior due to non-psychiatric causes have been ruled out.
“(3) The physical examination required to be provided to each person who remains at a receiving or treatment facility for more than 12 hours must include:
(a) A determination of whether the person is medically stable; and
(b) A determination that abnormalities of thought, mood, or behavior due to
non-psychiatric causes have been ruled out.”
It is medically known that there is a very real possibility that what seems to be a psychiatric problem can be caused by some physical illness with more than 100 medical disorders having been documented to mimic mental illness symptoms.
There are many different physical disorders that may lead a doctor to misdiagnose someone as having depression or bi-polar disorder such as influenza, infectious mononucleosis, viral pneumonia, cancer, sleep apnea and thyroid disease to name just a few.
Ideally this examination would be by a non-psychiatric and independent medical doctor and documented as having been administered to rule out non-psychiatric causes of thought, mood or behavior including the following tests to rule out physical ailments that can present as mental illness:
- sTSH (thyroid test)
- CBC (complete blood count)
- SGOT (liver function test)
- Serum albumin
- Serum calcium
- Vitamin B12
- Urinalysis
- 12 panel drug test
Question: Does a patient have a right to say what treatment they do or do not want to receive?
Answer: Florida Statute 394.459, Rights of patients, Section (2) RIGHT TO TREATMENT, Subsection (e) states:
“(e) Not more than 5 days after admission to a facility, each patient shall have and receive an individualized treatment plan in writing which the patient has had an opportunity to assist in preparing and to review prior to its implementation. The plan shall include a space for the patient’s comments.”
However, if you truly want to ensure that your wishes are respected, you should complete a Mental Health Advance Directive. This form can be downloaded from the Department of Children and Families at this link – Mental Health Advance Directive. You may also be interested in attending one of our workshops on Mental Health Advance Directives. These workshops are delivered by an attorney and are free of charge. For more information please call 727-442-8820.
Question: What is Express and Informed Consent?
Answer: Florida Statute 394.459, Rights of patients, Section (3), RIGHT TO EXPRESS AND INFORMED PATIENT CONSENT, Subsection (a)2. states:
“2. Before giving express and informed consent, the following information shall be provided and explained in plain language to the patient, or to the patient’s guardian if the patient is 18 years of age or older and has been adjudicated incapacitated, or to the patient’s guardian advocate if the patient has been found to be incompetent to consent to treatment, or to both the patient and the guardian if the patient is a minor: the reason for admission or treatment; the proposed treatment; the purpose of the treatment to be provided; the common risks, benefits, and side effects thereof; the specific dosage range for the medication, when applicable; alternative treatment modalities; the approximate length of care; the potential effects of stopping treatment; how treatment will be monitored; and that any consent given for treatment may be revoked orally or in writing before or during the treatment period by the patient or by a person who is legally authorized to make health care decisions on behalf of the patient.”
This simply means that a person, or the person’s guardian, is to be told, among other things:
- the reason for admission or treatment;
- the proposed treatment;
- the purpose of the treatment to be provided;
- the common risks
- the benefits
- the side effects
- alternative treatment;
- the approximate length of care;
- the potential effects of stopping treatment;
- how treatment will be monitored;
- and that any consent given for treatment may be revoked orally or in writing before or during the treatment period by the patient or by a person who is legally authorized to make health care decisions on behalf of the patient
Question: Does a parent/guardian have the right to express and informed consent to treatment if a patient is a minor?
Answer: Yes.
Florida Statute 394.459, Rights of patients, Section (3), RIGHT TO EXPRESS AND INFORMED PATIENT CONSENT, Subsection (a)1. states:
“(a)1. Each patient entering treatment shall be asked to give express and informed consent for admission or treatment. If the patient has been adjudicated incapacitated or found to be incompetent to consent to treatment, express and informed consent to treatment shall be sought instead from the patient’s guardian or guardian advocate. If the patient is a minor, express and informed consent for admission or treatment shall also be requested from the patient’s guardian. Express and informed consent for admission or treatment of a patient under 18 years of age shall be required from the patient’s guardian, unless the minor is seeking outpatient crisis intervention services under s. 394.4784. Express and informed consent for admission or treatment given by a patient who is under 18 years of age shall not be a condition of admission when the patient’s guardian gives express and informed consent for the patient’s admission pursuant to s. 394.463 or s. 394.467.”
Question: Does a patient have the right to communicate to their attorney, family and/or report alleged abuse?
Answer: Yes, but there are restrictions.
The law covering this is Florida Statute 394.459, Rights of patients, Section (5) COMMUNICATION, ABUSE REPORTING, AND VISITS, Subsections (c), (d) and (e) and it can be found by clicking here.
In our viewpoint, the important points to know are that :
- A person does have the right to communicate freely and privately with persons outside the facility unless it is determined that such communication is likely to be harmful to the person or others
- A telephone that allows for free local calls and access to a long-distance service is to be made available as soon as reasonably possible
- The telephone shall be readily accessible to the patient and shall be placed so that the patient may use it to communicate privately and confidentially.
- Facility rules on the use of the telephone may not interfere with a patient’s access to a telephone to report abuse
- Each patient shall be allowed to receive, send, and mail sealed, unopened correspondence
- No patient’s incoming or outgoing correspondence shall be opened, delayed, held, or censored by the facility unless there is reason to believe that it contains items or substances which may be harmful to the patient or others
- Each facility must permit immediate access to any patient, subject to the patient’s right to deny or withdraw consent at any time, by the patient’s family members, guardian, guardian advocate, representative, Florida statewide or local advocacy council, or attorney, unless such access would be detrimental to the patient
“If a patient’s right to communicate or to receive visitors is restricted by the facility, written notice of such restriction and the reasons for the restriction shall be served on the patient, the patient’s attorney, and the patient’s guardian, guardian advocate, or representative; and such restriction shall be recorded on the patient’s clinical record with the reasons therefor. The restriction of a patient’s right to communicate or to receive visitors shall be reviewed at least every 7 days. The right to communicate or receive visitors shall not be restricted as a means of punishment.”
- Each facility shall establish reasonable rules governing visitors, visiting hours, and the use of telephones by patients in the least restrictive possible manner.
- Patients shall have the right to contact and to receive communication from their attorneys at any reasonable time.
- Each patient receiving mental health treatment in any facility shall have ready access to a telephone in order to report an alleged abuse.
- The facility staff shall orally and in writing inform each patient of the procedure for reporting abuse and shall make every reasonable effort to present the information in a language the patient understands.
- A written copy of that procedure, including the telephone number of the central abuse hotline and reporting forms, shall be posted in plain view.
Question: Does the family or Representative of a patient, who was sent for involuntary examination have to be notified?
Answer: Yes, according to Florida Statute 394.4599 Notice, a facility is required to give prompt notice of the whereabouts of an adult who is being involuntarily held for examination to the individual’s guardian, guardian advocate, health care surrogate or proxy, attorney or representative, by telephone or in person within 24 hours after the individual’s arrival at the facility. These contact attempts are to be documented in the individual’s clinical record and begun as soon as reasonably possible after the individual’s arrival.
In the case of a child, a facility is required to give notice of the whereabouts of a minor who is being involuntarily held for examination to the minor’s parent, guardian, caregiver, or guardian advocate, in person or by telephone or other form of electronic communication, immediately after the minor’s arrival at the facility.
However, the facility may delay notification for no more than 24 hours after the minor’s arrival if the facility has submitted a report to the central abuse hotline based upon knowledge or suspicion of abuse, abandonment, or neglect and if the facility deems a delay in notification to be in the minor’s best interest.
Question: What are the criteria used for involuntary examination, a Baker Act?
Answer: Florida Statute 394.463, Involuntary examination, states:
(1) CRITERIA.—A person may be taken to a receiving facility for involuntary examination if there is reason to believe that the person has a mental illness and because of his or her mental illness:
(a)1. The person has refused voluntary examination after conscientious explanation and disclosure of the purpose of the examination; or
2. The person is unable to determine for himself or herself whether examination is necessary; and
(b)1. Without care or treatment, the person is likely to suffer from neglect or refuse to care for himself or herself; such neglect or refusal poses a real and present threat of substantial harm to his or her well-being; and it is not apparent that such harm may be avoided through the help of willing family members or friends or the provision of other services; or
2. There is a substantial likelihood that without care or treatment the person will cause serious bodily harm to himself or herself or others in the near future, as evidenced by recent behavior.
Emphasis has been added to show the key parts of these criteria.
Full Text of the Mental Health Law for Florida: The Baker Act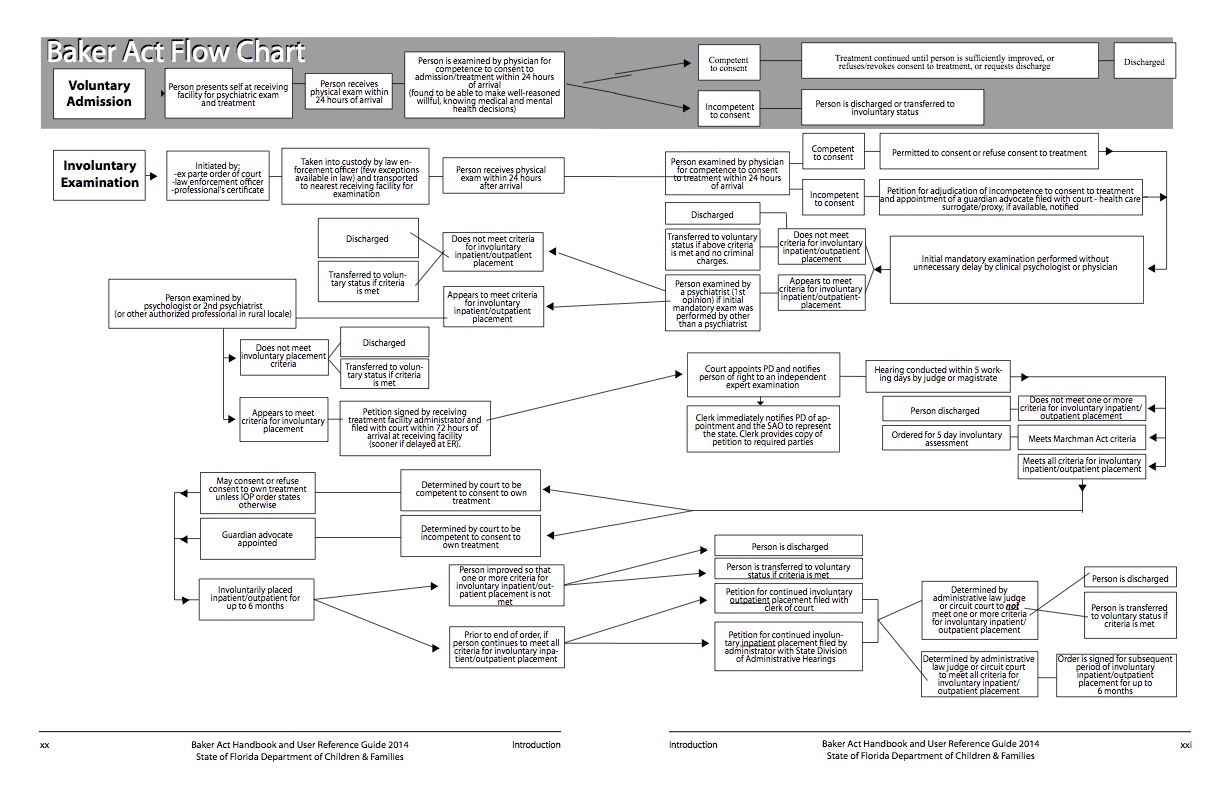 Download Baker Act Flow Chart
Download Baker Act Flow Chart

0 Comments
Trackbacks/Pingbacks